Bladder weakness after birth
8-minute read
What is urinary incontinence?
Urinary incontinence describes any accidental or involuntary loss of urine from the bladder. Incontinence can range in severity from a small leak to a complete loss of bladder control. Thankfully, there are ways to improve and even cure urinary incontinence. Seeking help early is recommended.
What causes urinary incontinence?
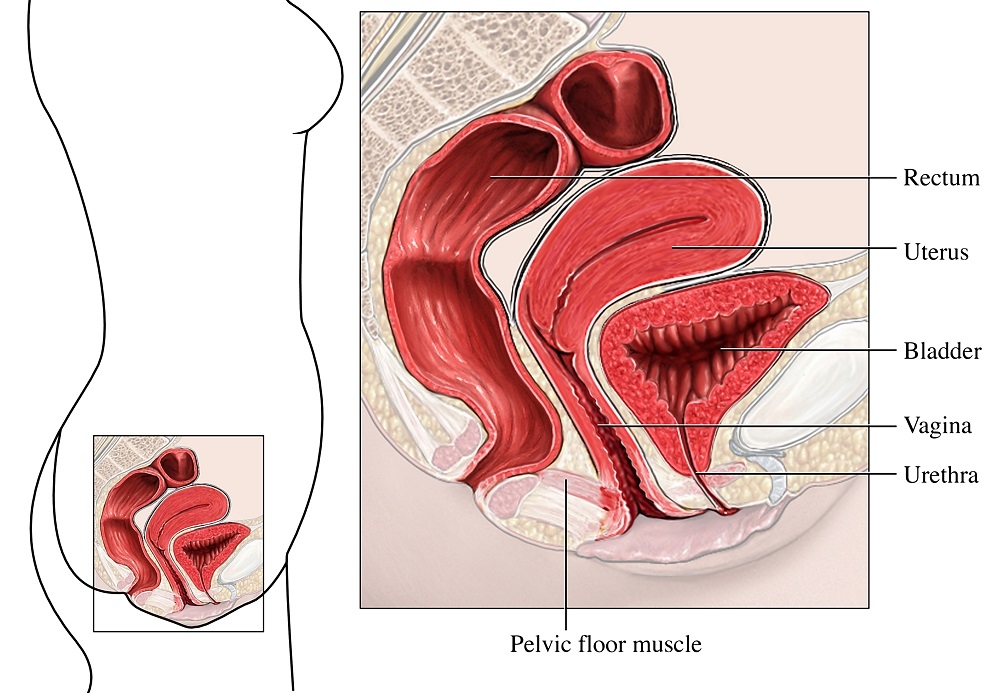
When you are pregnant, you produce hormones that stretch the muscles and tissues that support the bladder, the bowel and the uterus. This group of muscles and tissues is called the pelvic floor.
When your baby moves down through your vagina to be born, your pelvic floor stretches and it remains stretched for some time.
The combination of hormones and stretched muscles means the muscles that control your bladder are weakened. This can lead to an accidental leak of urine.
How common is urinary incontinence?
Leaking urine (called ‘urinary incontinence’) after childbirth is very common. One in 3 women who have had a baby may experience leakage at some point.
Some new mother may leak urine when they laugh, sneezes, coughs or exercises. This is known as stress incontinence.
You are more likely to develop stress incontinence after birth if you:
- have bladder or bowel problems before pregnancy – they are likely to get worse after the birth
- bladder problems during the pregnancy
- are having your first baby
- are having a large baby
- have a long labour, especially a long second stage of labour
- have a difficult delivery, such as needing stitches, tearing, or needing a vacuum cup or forceps during the delivery
Women who have a caesarean can also develop bladder problems. Having a caesarean can reduce the risk of severe incontinence from 10% to 5% for the first baby, but after the third caesarean women are just as likely to develop bladder problems as women who give birth vaginally.
When should I see my doctor?
Most women who leak urine after childbirth find that it goes away in the first few weeks, as the stretched muscles and tissues recover.
However, for some women it can take months while others find their pelvic floor never recovers fully.
If you are experiencing urine leakage, you can talk to your, doctor, maternal and child health nurse, continence nurse or a women’s physiotherapist. Remember dealing with it early can reduce the risk of it becoming a life-long problem.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
How is urinary incontinence treated?
The treatment will depend on what kind of incontinence you have and how severe it is.
Straight after birth, you will need to give the pelvic floor time to recover. Ice the perineal area for the first few days and have plenty of rest.
Then you can start with gentle pelvic floor contractions while you are lying down. Hold for 3 seconds, rest for 15 seconds, and repeat 3 times. Try to build up longer holds when you can. Doing these exercises may help prevent longer term bladder problems.
Simple changes to your lifestyle may also help, such as losing your pregnancy weight, eating more fibre, drinking more water and lifting less.
If your urinary incontinence doesn’t get better, talk to your doctor. They may refer you to another specialist. Longer term treatments for bladder weakness are exercises, medication or surgery.
Pelvic floor exercises
The muscles around the bladder, bowel and uterus can be exercised, toned and trained like any other muscles in the body. Doing this before, during and after pregnancy will help prevent urinary incontinence during pregnancy and after the birth of your baby. They’re easy to do, in any place and at any time.
Here’s an example:
- Breathe in and breathe out.
- Pull the pelvic floor muscles up and in as though you are trying to stop yourself from urinating.
- Hold the squeeze for 10 seconds while breathing normally.
- Relax and repeat in 10 seconds.
- Repeat the squeeze and release 10 times.
- Do this exercise 3 times a day.
The Continence Foundation of Australia have produced this video on how to do pelvic floor exercises:
You can also find out more about pelvic floor strength on the Jean Hailes website.
Bladder training
When you’re pregnant, your growing baby puts pressure on your bladder. This causes the bladder to feel full more quickly than usual, meaning you need more frequent trips to the toilet.
After your baby’s birth, it is a good idea to retrain your bladder. You can do this by trying to hold off from going to the toilet, until your bladder is full.
Medication
If you have urge incontinence, or an overactive bladder, medication can help to relax the bladder muscles.
Surgery
If all else fails, surgery might be an option for some women. Talk to your doctor about what's best for you.
Emotional wellbeing
Urinary incontinence can affect not only your physical health but also your emotional health and general wellbeing. For some women this complication may also be linked to an experience of birth trauma. If you find you are experiencing low mood or are concerned, you are not alone. There are service available to support you.
Living with urinary incontinence
Urinary incontinence can, unfortunately, become a long-term problem for some women. Here are some tips that may help if you are living with it:
- use incontinence pads, which are made for urine leakage, rather than sanitary pads
- take a change of underwear or set of clothes when you go out
- know where toilets are located so you can find them quickly (there are smartphone apps to help you do this)
- cross your legs when sneezing or laughing
- modify your exercise routine to avoid high impact exercises such as jumping
What can I do to prevent bladder problems after birth?
There are some simple steps you can take during pregnancy to help prevent incontinence.
- Drink 6 to 8 cups of fluid a day, unless your doctor tells you otherwise. Avoid drinks containing sugar or caffeine, as these can irritate the bladder.
- Eat a high fibre diet with 2 pieces of fruit, 5 serves of vegetables and 5 serves of cereals/bread per day.
- Make sure you have a healthy weight.
- Stop smoking.
- Exercise for at least 30 minutes most days (see below).
- Do regular pelvic floor exercises.
- Go to the toilet when you have the urge to open your bowels (poo).
- Sit properly on the toilet.
- Avoid constipation, as this strains your pelvic floor muscles.
- Don’t go to the toilet ‘just in case’.
- See your doctor straight away if you have a urinary tract infection.
It’s also important to exercise safely while you are pregnant and after the birth to avoid incontinence. Ideal exercises are walking, low impact aerobics, water aerobics, cycling on a stationary bike, swimming, light weight training or pregnancy exercise classes. To protect your pelvic floor, avoid:
- heavy weights
- high impact or jerky movements
- bouncing
- contact sports
- excessive twisting and turning activities
- exercises that require you to hold your breath
- exercises that require sudden changes of direction or intensity
- exercises that make you use one leg more than the other, or lifting your hip while you are on your hands or knees
- exercises that involve standing on one leg for a period of time
- activities involving sudden changes in intensity
- exercises that increase the curve in your lower back
Where can I go for more advice and support?
Speak to your doctor or midwife or call the National Continence Helpline on 1800 33 00 66 for more information and support.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022