Short cervix in pregnancy
7-minute read
Key facts
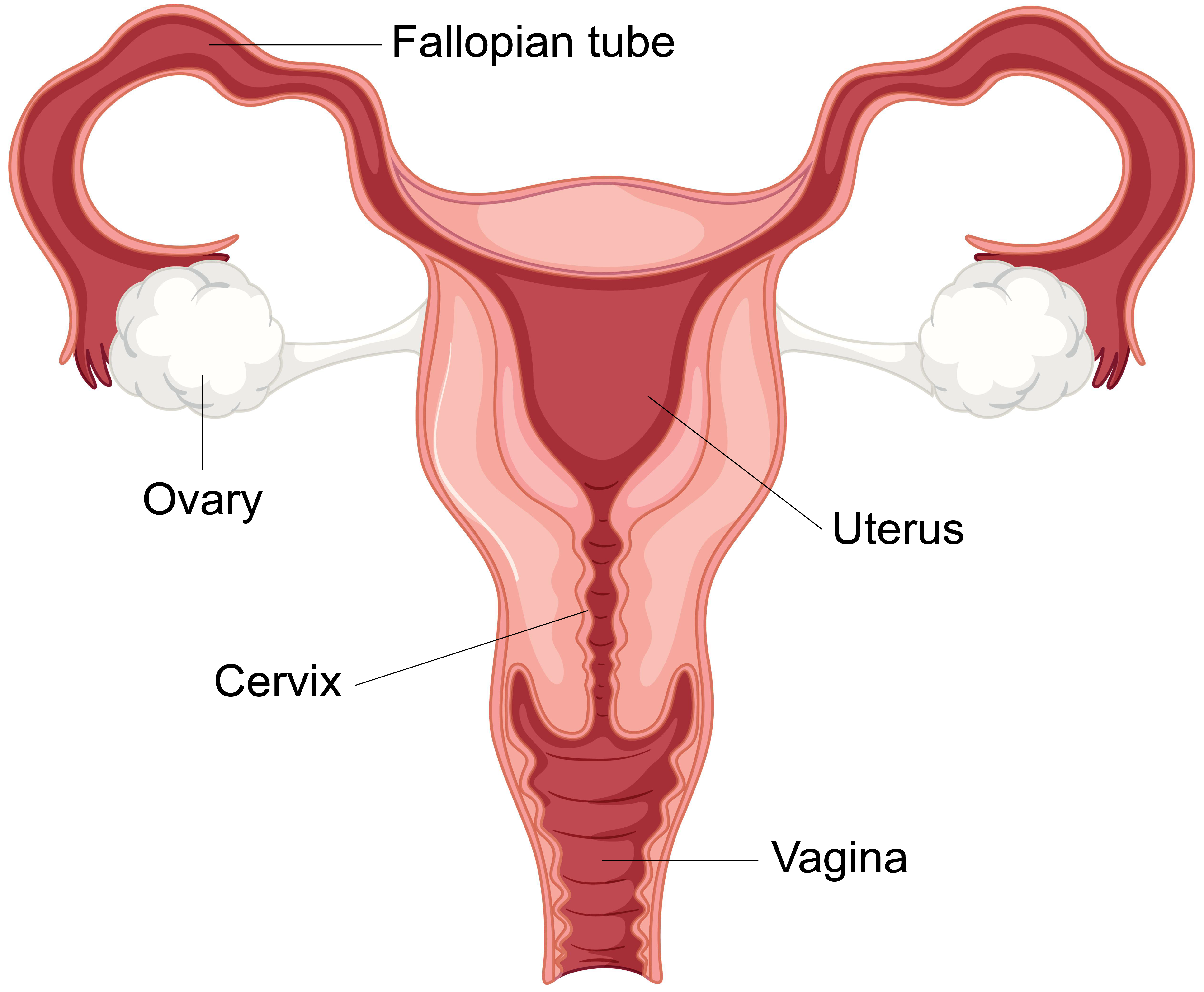
- The cervix is part of the female reproductive system and is found at the lower part of the uterus connecting to the vagina.
- A short cervix during pregnancy increases the chance of having a preterm (early) birth.
- Risk factors associated with having a short cervix include previously having a preterm birth or previously having a procedure on your cervix where a part of your cervix was removed.
- A short cervix is diagnosed using ultrasound.
- A short cervix can be managed during pregnancy with rest, progesterone medicine or a procedure called cervical cerclage.
What is the cervix?
The cervix is part of the female reproductive system and may be referred to as the ‘neck’ of your uterus. It is a muscular channel that connects the body of your uterus with your vagina. The cervix is usually around 3cm long and is made up of a central channel with an internal and external opening. It plays an important role in conception (becoming pregnant) and pregnancy. Your cervix makes mucus that helps to transport sperm from the vagina. It also keeps the uterus closed during pregnancy. During labour, the cervix relaxes and slowly opens.
What does it mean to have a short cervix during pregnancy?
The length of your cervix during pregnancy relates to the chance of you having a preterm (early or premature) birth. A short cervix is one that is less than 25mm (2.5cm) long at around 20 weeks of pregnancy. The shorter your cervix, the higher the risk of an early birth (earlier than 37 weeks pregnancy).
Most women with a short cervix still give birth on time, but if you have a higher-than-average risk of having your baby early, it is important to know this ahead of time, before labour begins, so that you and your health team can be prepared. Your health team may also suggest treatments to help reduce this risk.
Some hospitals or clinics measure cervical length routinely at around 20 weeks of pregnancy. Other places only measure cervical length if you have risk factors for preterm birth or if you have particular symptoms such as preterm contractions.
Are there risk factors for having a short cervix?
There are some risk factors linked with having a short cervix.
These risk factors include:
- previous preterm birth
- previous procedure on your cervix in which a small part of your cervix was removed
- previous cervical trauma including cervical tearing during labour or dilation and curettage (D&C)
How is a short cervix diagnosed?
A short cervix can be diagnosed using ultrasound.
Your doctor may do a transabdominal ultrasound (an ultrasound done on your tummy) in the middle of your pregnancy if you are at low risk of having a short cervix and have a singleton pregnancy (a pregnancy with one baby in your uterus). If your cervix is shorter than expected on the transabdominal ultrasound or your doctor has difficulty seeing your cervix properly on the transabdominal ultrasound, they may suggest doing a transvaginal ultrasound (an ultrasound done internally, through your vagina). The cervix can be seen better on a transvaginal ultrasound.
If you are at a high risk of having a short cervix, your doctor may suggest doing a transvaginal ultrasound to see your cervix more clearly and to measure the length of your cervix more accurately.
How is a short cervix managed during pregnancy?
There are different approaches to managing a short cervix during pregnancy. Your doctor may suggest using progesterone to reduce the risk of preterm birth. This medication can be given in the form of a small progesterone tablet, placed directly into your vagina or anus (bottom).
Cervical cerclage is another technique to help prevent pre-term labour that occurs because of a short cervix. It involves minor surgery that places a stich in the cervix. Your doctor may suggest this treatment if you have a singleton pregnancy and have a short cervix. Cervical cerclage is often recommended if you have previously had a premature birth or a pregnancy loss during your second trimester, or if your cervix continues to get shorter despite using progesterone daily. Your health team may also recommend this procedure if your cervix is very short (less than 10mm) in the second trimester.
In some cases, bed rest and admission to the hospital may also be recommended.
Are there risks to me or my baby if I have a short cervix?
While most women with a short cervix give birth on time, they are more likely to give birth early. Premature birth is the leading cause of newborn morbidity (illness) and mortality (death) worldwide. Premature birth can also lead to long-term health problems later in life. For this reason, it’s best to have a short cervix diagnosed early, so that you can be treated and monitored, and take steps towards preventing a premature birth.
Resources and support
As well as asking your doctor or nurse for advice, you can get help and information from:
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.
- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AEST).
- ForWhen — 1300 24 23 22 (Monday to Friday, 9.00am to 4.30pm)
- Gidget Foundation — online and telehealth support — 1300 851 758
- Beyond Blue — 1300 22 4636

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2023




