Perineal tears
14-minute read
Key facts
- Perineal tears are an injury to the skin or muscle between the vagina and anus (perineum).
- Perineal tears are classified in degrees from 1 to 4, depending on which layer of skin, muscle and other soft tissues has been affected.
- Depending on the type of tear, you may or may not need stitches.
- Women having their first baby, an instrumental delivery or a large baby are more likely to have a perineal tear.
- More serious perineal tears can extend into the muscle and skin of the anus, these tears are best repaired surgically in an operating theatre.
What is a perineal tear?
A perineal tear is a laceration of the skin, muscles and other soft tissues that separate the vaginal opening and the anus (back passage) also referred to as your perineum — the area between the vagina and anus. During labour, the skin and muscles between the vagina and anus stretch so the baby can be born. Sometimes the area gets torn, which results in a perineal tear.
What are the different types of perineal tears?
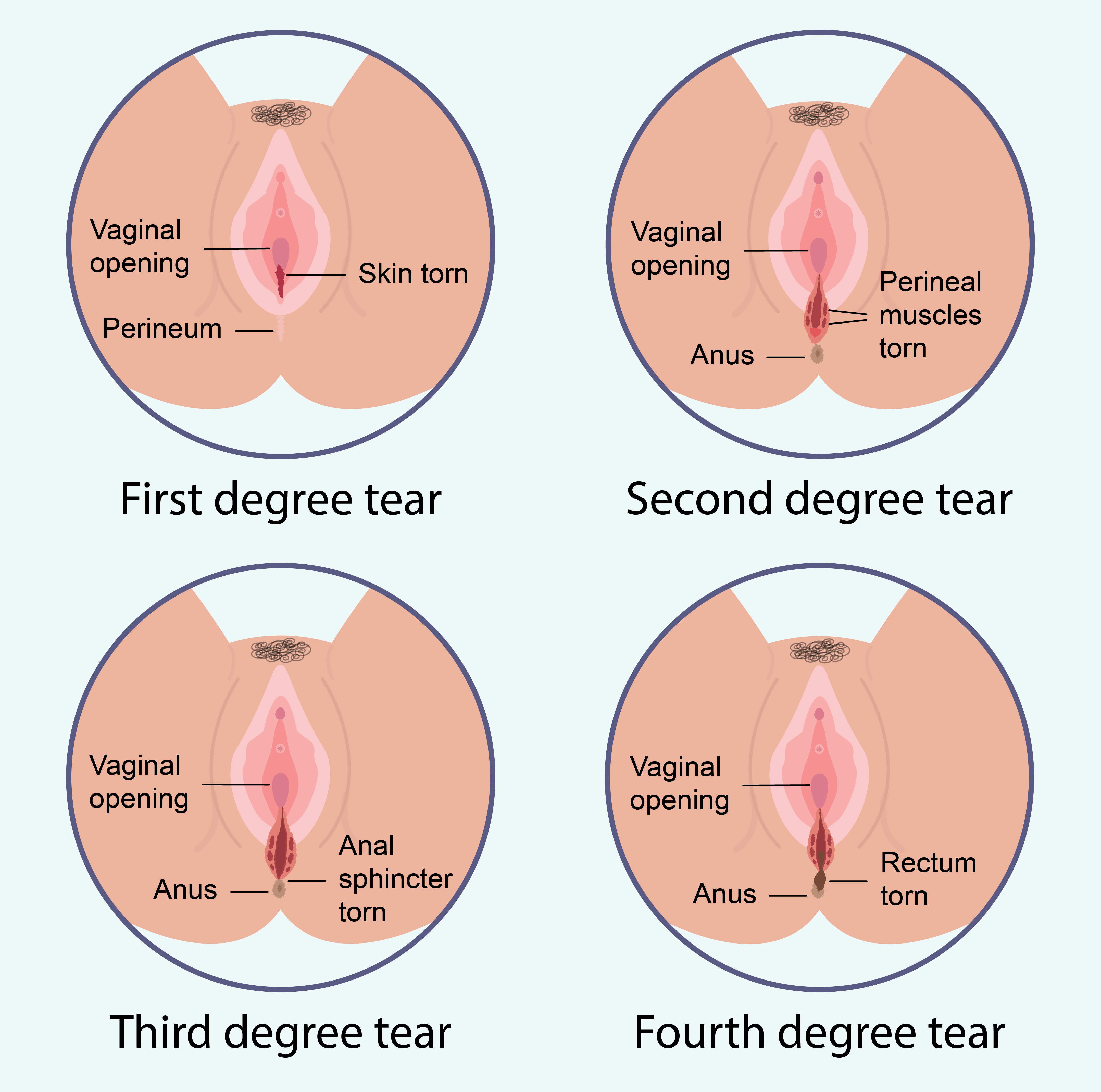
Perineal tears are graded from 1 to 4, depending on the severity and which tissue is affected.
First degree tears are small and skin-deep and can often heal without stitches.
Second degree tears are deeper and affect the muscles of the perineum. Stitches are usually recommended. Although occasionally a small second-degree tear can heal well without suturing.
A third-degree tear extends downwards from the vagina through the deeper muscles to the anal sphincter (the part that keeps the anal canal closed).
A fourth-degree tear affects the lining of the anus or rectum.
| Type of tear | Where it occurs | Treatment |
|---|---|---|
| First degree | Skin of the perineum or labia | May need stitches |
| Second degree | Muscles of the perineum | Usually needs stitches |
| Third degree | Muscles controlling the anus | Surgical repair |
| Fourth degree | Lining of the anus | Surgical repair |
What is the difference between a perineal tear and episiotomy?
A perineal tear happens when the skin between the vagina and anus tears.
An episiotomy is an intentional incision made by a doctor or midwife. An episiotomy is done using surgical scissors, when the perineum has stretched and the baby’s head is crowning.
What makes a perineal tear more likely?
A perineal tear is more likely if:
- this is your first baby
- you are of Southeast Asian background
- you have previously had a third or fourth degree perineal tear
- your baby weighs more than 4kg (9lb) or is in a position with their back against your back (posterior)
- your baby’s shoulders become stuck during birth
- you require forceps or other instruments to assist your birth
How can I reduce my chance of a perineal tear?
During the later stages of pregnancy, regular pelvic floor exercises and perineal massage from 35 weeks, may help protect your perineum and prevent perineal injury.
It is also a good idea to talk to your midwife or doctor about your risk factors and the strategies used in your chosen hospital or birth centre to reduce the likelihood of sustaining a serious tear.
Questions you might want to ask your healthcare provider
- What can we do to reduce the chances of me sustaining a significant tear?
- Does your hospital have a policy in place to reduce incidences of third and fourth degree tears? If so, how will this influence my care?
- Are we able to look at possible risks in my circumstance?
Will I need stitches if I have a perineal tear?
First- and second-degree perineal tears are common and most heal well either naturally or with stitches. Depending on the location and extent of the tear, you may need stitches; these are done soon after the baby’s birth. Your doctor or midwife will be able to advise what is right for you based on their assessment of the type of tear sustained and your preferences.
What happens if I have a tear?
After your baby is born, your doctor or midwife will check your perineum for any tears or grazes. Sometimes it’s obvious during birth that the perineum has torn, but not always. This is why it’s important to be carefully checked after your baby is born.
If a tear is identified, once the severity has been assessed, your doctor or midwife will discuss the best mode to repair the tear. You should be given enough information to be able to provide your informed consent. Any decision to repair a tear or not will be made in consultation with you.
Most first- and second-degree tears can be repaired in the same room where you gave birth. If you had an epidural, this will keep running to ensure adequate pair relief while the sutures are being put in. Otherwise, a local anaesthetic will be injected into your perineum near the affected area to numb it before suturing begins.
To reduce the chance of incontinence, all third- or fourth-degree tears are recommended to be repaired surgically. This is often performed in an operating theatre where there is good access to pain relief and all the lighting and tools the surgical team need to repair the sphincter and perineum successfully.
Once your doctor or midwife has finished stitching, they will usually offer you pain-relief medication and place a pad and some ice on your perineum to help with any swelling.
How long will it take to heal from a perineal tear?
It is normal to feel pain or soreness around the tear or cut for 2 to 3 weeks after giving birth, especially when walking or sitting. The skin stitches usually dissolve within 3 weeks and full healing can take up to 6 to 8 weeks.
What can help my recovery after having a tear?
There are a few things you can do to help support the healing of your perineal area. Keep in mind that everyone is different and it is always best to follow the instructions of your healthcare team:
- Try to rest as much as possible and lie on your side if you can.
- Avoid positions and activities that place pressure on the muscle or restrict blood flow to the area, like sit-ups, lifting and high impact exercise.
- Keep the tear clean and dry — shower daily and gently pat the area dry.
- Avoid using any cream ointments or powder on the area, unless you’ve been advised to by your healthcare provider.
- Change your pads frequently.
- Start gentle pelvic floor muscle exercises 2 to 3 days after your baby’s birth, or when it’s comfortable for you to do so.
- Avoid becoming constipated, drink plenty of water and try to eat a diet rich in fibre (fruit, vegetables and wholegrains).
- Take your time when emptying your bladder and bowel and avoid pushing or straining.
- Use a foot stool or lift your heels up so that your knees are above your hips when you’re sitting on the toilet.
- Try to keep well hydrated so your urine is less concentrated. This can help reduce stinging.
- Try leaning forward on the toilet when you pass urine, this will keep the urine away from the tear and reduce stinging.
Learn more about scar healing and recovery.
When can I have sex?
There is no standard waiting period before women can resume sex after having a baby. However, most maternity care providers recommend waiting until after the bleeding has stopped and the tear has healed, and once you feel interested in having sex. For many birthing mothers, this happens within 1 to 3 months after having their baby.
Ultimately, you should only resume having sex when you feel ready to do so.
Can I have a vaginal birth in the future?
Some women are advised not to have a vaginal birth again if they had a third or fourth degree perineal tear with a previous baby. This is different for each person and will vary depending on your circumstance and preferences. Be guided by your doctor or maternity care provider about what is right for you.
When should I see a doctor?
Most women are advised to have a postnatal check 6 weeks after their baby’s birth.
See your doctor earlier if you are concerned about how your perineum is healing or if you have other concerns with your vagina, bladder or bowel after birth, such as:
- you develop a temperature
- you notice an unusual smell or discharge from the tear
- your perineum becomes inflamed, swollen and red
- your perineal tear is still causing you pain after 2 to 3 weeks
- you cannot control your bowels or passing wind
- sex is painful for you
- you have a heavy, dragging sensation in your vagina
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
Who can I speak to if I'm not satisfied with my healthcare?
If you aren’t satisfied with your healthcare, there are many people you can speak to, including:
- your doctor or midwife
- the health complaints agency or health department in your local state or territory
- the Australian Health Practitioner Regulation Agency (AHPRA), if you have a concern about the unsafe behaviour or practice of a registered health practitioner
- the National Health Practitioner Ombudsman
If you aren’t sure about something that happened to you, especially during labour, birth or in an emergency, it’s a good idea to ask your doctor or midwife for a debrief. This is an opportunity to ask questions after an event, so that you better understand what happened.
Resources and support
- Talk to your doctor, midwife or obstetrician.
- The Continence Foundation of Australia offers information and support to people with bowel and bladder problems. You can call the helpline on 1800 33 00 66 between 8am and 8pm (AEST), Monday to Friday.
- Visit Australasian Birth Trauma Association for information and support, including peer-to-peer support.
- Visit PANDA (Perinatal Anxiety and Depression Australia) for information and support after a traumatic birth. You can call the PANDA national helpline on 1300 726 306 (Monday to Friday 9am to 7:30pm AEST).
- ForWhen on 1300 24 23 22 (Monday to Friday 9am to 4:30pm).
- Beyond Blue on 1300 22 4636.
- Call the National Domestic Family and Sexual Violence Counselling Service on 1800 RESPECT or 1800 737 732 (24 Hours a day, 7 days a week).

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2023